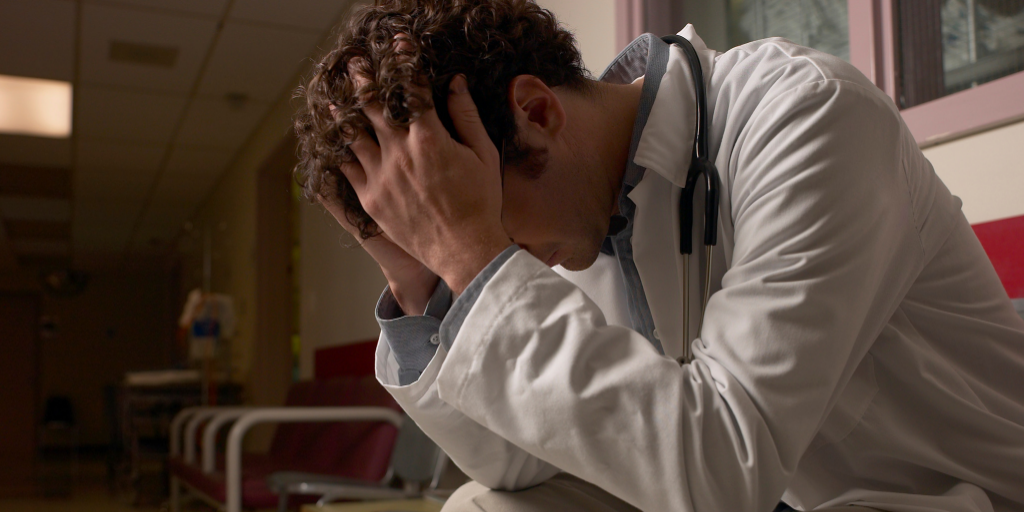
In recent years, there’s been a flood of literature regarding the malady of physician burnout. There are those harrowing statistics you hear when you’re in my line of work — 54 percent of American doctors and 64 percent of American primary care doctors exhibit at least one symptom of burnout.
However, no amount of data or statistics can shed light on the emotional, mental, and physical toll American physicians undergo when in the throes of burnout. Burnout is a cancer, one that is gradually — yet methodically — eroding our physicians’ sense of being. Without a cure, or cures, we’ll risk losing everything we’ve gained in pursuit of the Triple Aim, that promising beacon of lower costs, greater access to care, and higher quality care.
As difficult as it can be to admit, I’ve suffered from burnout. However, I believe that as physicians we must be honest and vulnerable about the ways we’re affected if we want to reform the system, curing the cause rather than treating the symptoms. I was a midcareer, busy primary care doctor all too familiar with the day-in, day-out tasks that monopolize nearly every second we aren’t with patients. I’d recently left a hospital system in favor of an independent practice, a change that I welcomed and championed yet still struggled to adapt. Perhaps the figurative straw that broke the camel’s back was my first malpractice lawsuit, an event that left me doubting my professional self-worth.
Epiphanies can be a bit of a cliche, but I have no doubts that I experienced one on that night in February. Thumbing through the latest issue of JAMA, I read Dr. Tait Shanafelt’s “Addressing Physician Burnout: The Way Forward.” In that moment, I was transformed; I was stunned; I was validated. I didn’t feel alone, outlandish, or selfish.
More importantly, I recognized feelings I had almost forgotten: empowerment, hope, and a sense of calling to improve the health and experience of my fellow physician community. I was frustrated that we hadn’t been there for one another, that we’d lost sight of those core beliefs and tenets that led us to medicine in the first place. Yet I was motivated, too. I was hopeful and determined to make a difference for my fellow doctors.
Shortly after this realization, I enrolled in Brown University’s Executive Master of Healthcare Leadership program, which I recently completed. This program challenged us to pinpoint a specific, critical challenge in healthcare then research and create a novel solution. Unsurprisingly, I selected physician burnout and spent the last 16 months brainstorming, researching, and formulating an evidence-based, actionable solution — one that is led, powered, and focused on physicians.
In the process, I had the honor of speaking with thought leaders and participating in existing burnout programs. I practiced all that I learned, allowing myself to be vulnerable with my classmates, many of whom were physicians. In doing so, I noticed the barriers the American healthcare system erects as well as the bridge through all of the chaos, inefficiency, and isolation. That bridge is made up of a community of our fellow physicians.
I’m happy to say that not only am I thrilled to be practicing medicine again and that I’ve rediscovered the joy of treating patients, but that I also have a new goal: combating burnout.
This series is designed to give a professional and personal look at the program I designed, one that I believe could alleviate much of the stress and lost opportunities burnout can cause. We’ll examine the ways in which the emotions that led us to medicine can, paradoxically, lead to burnout. Service, excellence, curative competence, and compassion are all wonderful values. However, they contain downsides that, if not handled carefully, jeopardize our patients’ and our own well-being.

Our doctors are based in your community, centered on your needs, and part of a national network that’s transforming healthcare.

Healthcare, handled.
You have enough on your plate. We make it easy to message your doctor, connect to on-demand virtual care, receive appointment reminders, refill prescriptions, and more.

Healthcare for the long haul.
You’re more than a set of symptoms. From pediatrics to adult needs, preventive programs to complex care – we’re here to support you on every step in your journey.

Our doctors do more.
You can enjoy personalized care without pricey fees. Our doctors take time to listen to your concerns, from wellness programs to chronic care management.


Healthcare, handled.
You have enough on your plate. We make it easy to message your doctor, connect to on-demand virtual care, receive appointment reminders, refill prescriptions, and more.

Healthcare for the long haul.
You’re more than a set of symptoms. From pediatrics to adult needs, preventive programs to complex care – we’re here to support you on every step in your journey.

Our doctors do more.
You can enjoy personalized care without pricey fees. Our doctors take time to listen to your concerns, from wellness programs to chronic care management.
Newsroom
inforMD Blog
Events
Presentations
The Break Room
Search Results
-
- Who We Support
- What We Offer
- About Us
- Careers
- Media
Looking for Coronavirus (COVID-19) information? View resources for patients.
Are you interested in finding out more about PRIVIA+?

Related Articles
How to Keep Your Patients From Skipping Mammograms
Kristin Schraa, MD, with Virginia Women’s Center shares how women’s health providers can encourage patients ...
3 Ways Healthcare Can Integrate Behavioral Health and Primary Care
Integrating behavioral health with primary care can lead to better patient outcomes — but how ...
How Can Physicians Support Postpartum Mental Health?
On average, 13 percent of mothers in the United States will develop symptoms of postpartum ...
Engaging Patients in Annual Mammograms
Studies show that a little over 66 percent of women aged 40 and older get ...
What Do Medicare-Aged Patients Want in Their Healthcare?
Within the next 20 years, 20 percent of Americans will be 65 or older. It ...
How Health Systems Grow Stronger With Privia Health
Discover how we helped Health First upgrade technology, align physicians, and accelerate toward value-based care. ...